Before I embarked on my second year of medical school, I wanted to try something different — an experience I probably wouldn’t attain during the medical school curriculum.
I have always had an inquisitive mind, hence research held a natural appeal. Research, at least to me, can be broadly categorized into two groups: dry lab and wet lab. I was already involved in the former, but was keen to give the latter a shot. An oncologist took me under his wing, and I was soon introduced to the world of lab-based, experimental research.
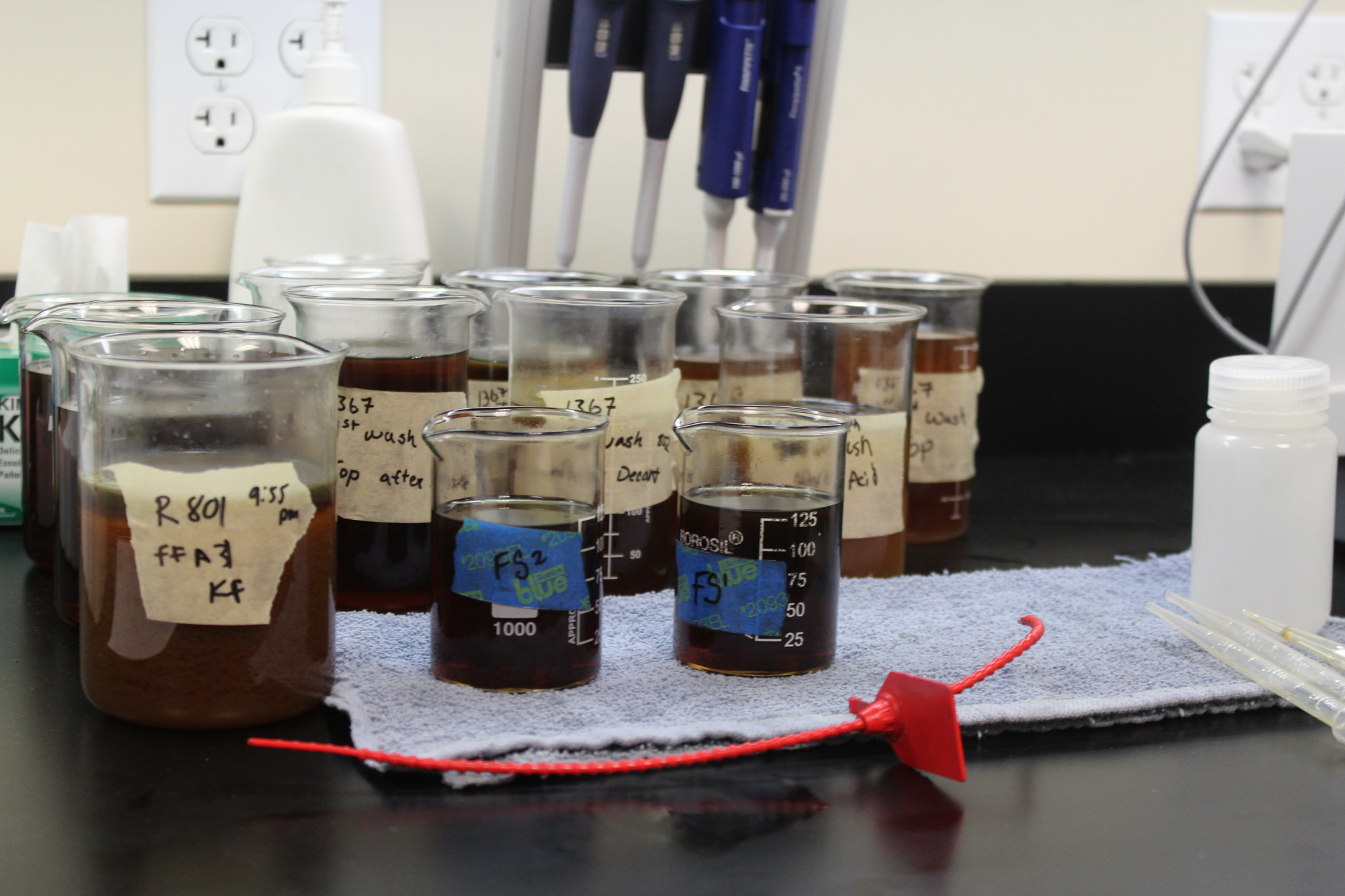
Coming from a background with literally no lab experience, it was undoubtedly a steep learning curve at inception. There was an avalanche of lab-based skills I needed to learn and understand. I was tasked to perform lymphoma research, but it wasn’t until a month later that I actually got to perform experimental work on lymphoma cells. The first month was humdrum but necessary. I had to complete multiple safety courses, practice micro-pipetting, and learn about the entire range of complex lab equipment and procedures such as the centrifuge, film development for western blots, and flow cytometry machine.
After one month, I was given my topic and tasked to draft the experimental protocol. In brief, I was investigating complement-mediated cytotoxicity of rituximab (anti CD20 monoclonal antibody) on lymphoma cell lines. Even though I had some prior knowledge about the cytotoxic mechanism, I had to perform an in-depth literature search to augment my understanding and look for existing experimental protocols that I could potentially adapt.
With a protocol in my armament, I thought I was confident and equipped enough to perform the experiment, until I realized that multiple roadblocks lay ahead of me. An initial protocol with six simple steps turned out to be twice as long after adding several intermediate steps that I had missed. There were other reagents that I had to add. For instance, staining the cells involved identifying the appropriate stain color, optimizing the concentration of the stain solution, incubating it for a period of time; it was not as simple as adding a reagent to a test tube of cells. Hence, it often took longer than expected to complete a single step, which resulted in me being late for the equipment bookings. Time management was the first lesson for me. It was quintessential for me to plan, in detail, the total amount of time I actually needed per step, with some degree of overestimation.
The road ahead was filled with pockets of ups and downs, albeit often the latter. There were many occasions on which experimental results contradicted my hypothesis – cells died when they were not supposed to; cells didn’t die when they were supposed to. When occasions like these arose, I went back to scrutinize every step in the protocol, to make sense of what could have possibly went wrong. But I soon realized that the things that seemed insignificant to me were the sources of the experimental failures. For instance, I had initially assumed that all serum types were similar in composition and purpose. However, the serum I had used was not viable for cell survival. Hence, I switched from commercial serum to human serum in subsequent experiments. The next road block came when my cells became unresponsive to rituximab. It was only much later on that I accidentally happened upon a paper, which stated that the particular cell line in my experiment was intrinsically resistant to the drug. These experimental failures served to teach me one very important lesson — to scrutinize the fine details and consider every possibility that could account for failures.
Lastly, I would like to underscore the significance of perseverance. I consider it to be the cornerstone of being a good scientist and researcher. Amidst the myriad of failures, I would have given up on continuing my experiments if I was devoid of it. Research can be a plodding process with multiple failures; but if you believe in your purpose and persevere, you will eventually reap the fruits of your labor.
I have always had an ardor for research, and I intend to pursue the Clinician-Scientist pathway. I am thankful for this lab experience, for it has opened my eyes to the unappealing — at least to most medical students —world of research. As mundane as it can be, I find both the process and end product meaningful to fellow scientists, doctors, and the society at large. This experience has not stifled my interest and passion for research and science; it has taught me instead the values that are essential for a scientist.
If you’re thinking of doing research or being a clinician-scientist, this is just my two-cents worth of lessons that I’ve personally picked up in my short five month stint thus far in the lab. Be humble. Be hungry to learn. Be careful to look out for details. And, most importantly, persevere despite how monotonous research can be.
Photo Credit: United Soybean Board