We are excited to publish the final contributor to this year’s Commencement Archive, Dr. Koh’s 2015 commencement speech to the Yale School of Medicine, “Finding your calling.”
Howard Kyongju Koh is the former United States Assistant Secretary for Health for the U.S. Department of Health and Human Services (HHS).
 Dr. Koh oversaw the HHS Office of Public Health and Science, the Commissioned Corps of the U.S. Public Health Service, and the Office of the Surgeon General. At the Office of Public Health and Science, he spearheaded programs related to disease prevention, health promotion, the reduction of health disparities, women’s and minority health, HIV/AIDS, vaccine programs, physical fitness and sports, bioethics, population affairs, blood supply, research integrity and human research protections.
Dr. Koh oversaw the HHS Office of Public Health and Science, the Commissioned Corps of the U.S. Public Health Service, and the Office of the Surgeon General. At the Office of Public Health and Science, he spearheaded programs related to disease prevention, health promotion, the reduction of health disparities, women’s and minority health, HIV/AIDS, vaccine programs, physical fitness and sports, bioethics, population affairs, blood supply, research integrity and human research protections.
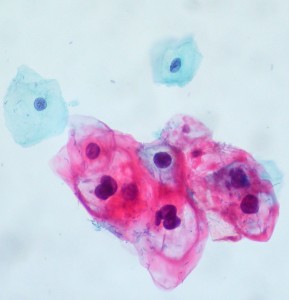
Dr. Koh graduated from Yale College and earned his medical degree from Yale University School of Medicine. He has earned board certification in four medical fields: internal medicine, hematology, medical oncology, and dermatology, as well as a Master of Public Health degree from Boston University.
Dr. Koh previously served as the Harvey V. Fineberg Professor of the Practice of Public Health, Associate Dean for Public Health Practice, and Director of the Division of Public Health Practice at the Harvard School of Public Health.
Dr. Koh begins his speech by advising students to find meaning and fulfillment in medicine, regardless of external expectations,
“Please listen carefully to your inner soul so that you can discover your own sacred calling. Doing so will help you express yourself, not just prove yourself. Doing so will help you determine in your life what is ultimate versus what is merely important.”
He continues by reminding students that patients will be teachers as well, and may be key factors in finding that calling,
“One way to learn more about meaning through your journey is to respect how your patients find meaning in their own. They can teach you in unexpected and profound ways. Sometimes the patients who will educate you the most will be the ones you couldn’t cure, no matter how hard you tried.”
He concludes and advises students to enjoy every step of the way,
“So please pay great attention to how you live your lives, not just as doctors, but as individual human beings.”
Visit the Medical Commencement Archive to read Dr. Koh’s full speech here