Beyond borders, beyond languages, and beyond our differences students across the world have united with a common purpose to serve and create a positive impact. With over 1000 students comprising more than 90+ countries, #Students_Against_COVID, a grassroots movement has served as the cornerstone for creation, purpose, fulfillment and fostered collaborations throughout the world allowing students to join forces in the fight against the COVID-19 pandemic.
The Power of Technology
The Spanish Flu or the 1918 pandemic over 100 years ago, vastly differs from the COVID-19 pandemic due to the availability of technology. Since then, there have been many advancements with new medical equipment and instruments to care for patients. Many cures for diseases or drugs that were impossible decades ago are now a reality due to the hard work and diligence of researchers in finding answers to the centuries’ old medical mysteries. During the Spanish flu pandemic, scientists could hardly imagine elucidating the nucleotide makeup of the virus, but with the advent of polymerase chain reaction (PCR) half a century later, in today’s technological landscape, within 2 weeks of a global emergency scientists were able to determine the sequence of the coronavirus genome. Within seconds, a text message from South Africa is transferred via the internet to Canada, and as such the spread of information and misinformation has appeared to be an added pandemic, namely the infodemic of the century.
Objectives of SAC, the Grassroots Movement
One of the core objectives of SAC in tackling the infodemic and the pandemic, has been to disseminate trustworthy information as quickly as possible and in as many languages to reach minorities, villages and people far away. From Pashto in Afghanistan, Turkish in Turkey, German in Austria, Hausa in West Africa, Yoruba in Nigeria to Lugada, the most prestigious language in Uganda, “the Pearl of Africa”, students have translated different COVID-19 campaigns.
The objective of the Global Health & Social Media Team has been to echo public health guidelines to stop the transmission of the infectious disease and to encourage those with symptoms of COVID-19 to seek medical assistance. Despite the socio-economic challenges for many without access to the internet, the major global health challenges the international community face will require an integrated, interdisciplinary approach addressing the political, cultural, legal, biological, and medical issues. Therefore acknowledging the role of technology in tackling the ongoing pandemic the team aims to eliminate avoidable disease, disability and death, while serving as an avenue of health promotion and disease prevention.
As such, important values, such as altruism, service in times of crisis, and solidarity with people around the world offered the chance, or opportunity of a lifetime to participate in the fight of this historic pandemic. Stemming from leadership’s most fundamental element to create a difference in the lives of others SAC therefore provided students with a platform to unleash their creativity and innovation necessary to navigate a crisis and to emerge from it healthy.” by Leah Sarah Peer
Additionally, with increased reliance on virtual platforms for connection and socializing, telehealth technologies for consultations, counseling sessions and physical examinations, physicians have been able to continue providing care while maintaining social distance. Similarly, educational institutions have transitioned to online remote learning where students and professors meet over interactive technologies such as Zoom and Google Meets for lectures. Medical students especially have had their clerk-ships suspended without direct patient contact while others have graduated early to serve as front-line clinicians. In this manner, technology has defied space and time, as it has not only exposed the fragility of humanity but also proved that technology is an integral part of our future evolution.
A Spark of Creativity & Innovation
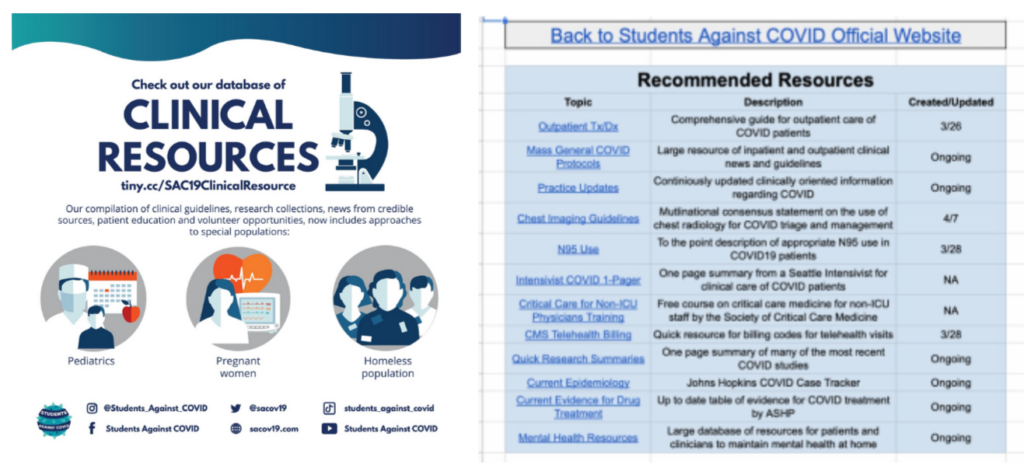
With more free time for students, as the usual commutes to school, scheduling of classes and extracurricular in person activities were all cancelled they were able to invest in themselves and even develop new hobbies. Within SAC, it was evident that despite the negative impacts on medical education, these exceptional times represented opportunities for change. Such an example is that of the Clinical Resources Team, that curated a database of clinical resources for health professionals to access COVID-19 & medical information. This volunteer experience among many highlighted the value of non-graded elective courses in furthering student’s knowledge while allowing them to participate in a movement greater than themselves. As such, important values, such as altruism, service in times of crisis, and solidarity with people around the world offered the chance, or opportunity of a lifetime to participate in the fight of this historic pandemic. Stemming from leadership’s most fundamental element to create a difference in the lives of others SAC therefore provided students with a platform to unleash their creativity and innovation necessary to navigate a crisis and to emerge from it healthy.
Besides making a difference, SAC provided a sense of community where friends soon became family. In isolation many were reminded of our collective values and collective history, emphasizing society at large rather than individual self-interest.
The Mental Health Team sparked the beginning of students inspiring one another, of sharing their own stories as well as becoming listeners as a crisis naturally triggers a range of physiological and psychological responses that are heightened under lock-down. The earlier trauma and abuse students faced often resurfaced as the lost sense of normalcy triggered grief with feelings of denial, anger and depression.
Bearing the consequences in mind, the Women’s Health Team of SAC drafted up a list of domestic violence hotlines per country for individuals afflicted by domestic violence. To them, having access to these resources during quarantine was vital and therefore have further created campaigns on sexual health, reproductive rights, maternal health and “The Period Project”, all aiming to raise awareness for the challenges girls and young women are faced with. Passionate about women’s health, to commemorate international breastfeeding week, educational material was prepared celebrating womanhood while promoting access to skilled breastfeeding counseling.
Advocating for Vulnerable Populations
Nonetheless, the #Students_Against_COVID community rarely sleeps and while students are taking care of themselves, and those around them, they are also actively advocating for vulnerable populations.
The Asylum Seeker’s & Refugees initiative within SAC aims to raise awareness about the predicament of minorities by creating infographics, and posters. Furthermore, underway is the curation of a database of World Organizations & Charities for donations so that donors have access to places where their funds are needed and may be used wisely. In a catastrophe such as that presently in Lebanon, the database gathers recognized Lebanese Non-Governmental Organizations (NGOs) providing humanitarian aid and emergency relief.
Additionally, bearing in mind the challenges of the COVID-19 pandemic, the team recognizes the plight of refugees suffering from human rights violations. Whether forced to leave their homes, their communities and their families, to find safety in another country, the Asylum Seekers & Refugees Team within SAC abides by the Universal Declaration of Human Rights (UDHR) to assure all human beings are treated with respect and dignity. Since, by definition, refugees are not protected by their governments, the international community steps in to ensure the individual’s rights and physical safety while monitoring and promoting respect for refugee rights. Although the newest edition to #Students_Against_COVID family, the team’s aim is to strengthen and broaden public information, education and involve members of the civil society in refugee, asylum seekers and migrants protection.
Reflecting on the Past Year & Moving Forward
Recognized for it’s positive contributions internationally, #Students_Against_COVID was awarded the Pollination Project grant, won 1st place in the DICE Foundation COVID-19 Innovation Challenge, as well as the 2021 CUGH Pulitzer Prize for Highest Impact Project, Video Submission.
Besides these accomplishments, currently in the works and set to launch late spring to early summer 2021, is the creation of a unique, Global Health Program: An interdisciplinary Overview. It’s aim is to cultivate a better understanding of Global Health amidst the COVID-19 pandemic and the program hopes to connect global health enthusiasts from around the globe, introducing students and young professionals to critical global health issues and ways to address or solve them.
As the crisis evolves, compassionate leadership entails the unified efforts of changemakers championing science in both local and international theaters. Although words may not adequately serve to express the work and dedication of this virtual agora, pushing boundaries to inspire, help and motivate people is at the centre of the #Students_Against_COVID movement!
To join SAC or to become a part of this ever expanding network of motivated youth, check out our website, find us on Instagram, Twitter, Facebook, LinkedIn, and Youtube.
About the Author
Leah Sarah Peer is a medical student at Saint James School of Medicine in Chicago and a graduate of Concordia University, Specialization in Biology, Minor in Human Rights in Montreal, Quebec, Canada. As a Core-Facilitator within Students_Against_COVID, Leah aims to foster belonging and inclusion to unify the movement and compassionately strives to empower others to make a difference.