“Illness is the night side of life, a more onerous citizenship. Everyone who is born holds dual citizenship, in the kingdom of the well and in the kingdom of the sick. Although we all prefer to use the good passport, sooner or later each of us is obliged, at least for a spell, to identify ourselves as citizens of that other place.”
– Susan Sontag, Illness as a Metaphor
Words are important. They allow us to meet on a common ground, to share experiences and learn from each other. They can evoke every emotion and open new friendships. They can also be therapeutic, and a way to fill the gap between doctor and patient.
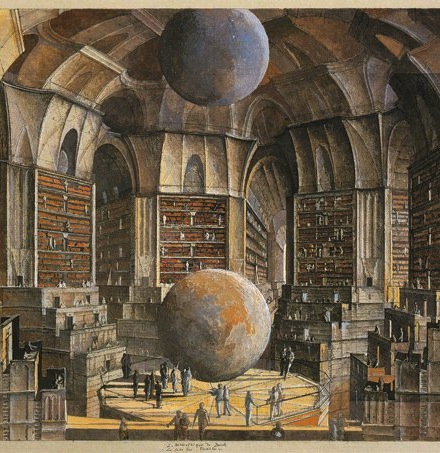
Pathographies, defined by the Oxford Dictionary as ‘the study of the life of an individual or the history of a community with regard to the influence of a particular disease or psychological disorder’, have become more popular over the years (1). Walk into any bookstore and you will eventually come across the healthcare corner: a small stack of books by people who have crossed the abyss into the land of ill health. Such stories speak of hope, love, loss, and despair as patients and their families come to terms with the sudden invasion into their lives. Treading through illness can be an isolating experience, filled with pain and uncertainty.
The Database of Individual Patient Experience is a UK-based charity that runs two websites: healthtalk.org and youthhealthtalk.org. It was created by Dr Ann McPherson, a GP who was diagnosed with breast cancer, but found that she had no one to talk to and share her experiences with. As a result, these websites are filled with patient’s experiences of their illnesses, how they coped, and their family’s reactions. Such websites can open a common ground for those who are suffering, those who are newly diagnosed, and the friends and family who may want to learn about how they can help.
“I am tired of hiding, tired of misspent and knotted energies, tired of the hypocrisy, and tired of acting as though I have something to hide.”
– Kay Redfield Jamison, An Unquiet Mind
How can they help us?
Pathographies are about putting the patient at the heart of healthcare and asking the question: can I truly understand what a person is going through if I have never suffered that ailment myself? By putting experiences into words a bridge is created, allowing those of us who work in healthcare to reach out that bit further. These stories can help us to take a step back from our jargon-filled lives; to not see the routine dialysis, but the precious hours spent with the husband; not the dry numbers of oxygen steadily increasing upon the hospital charts, but the feeling of accomplishment when one is able to take that first breath unaided. Illness is not just a list of problems that need to be crossed off. It is a continuous process filled with dark corners and dead ends.
In an increasingly globalized world, an appreciation of the cultural diversity lying upon our doorsteps is ever more needed. Everyone experiences illness in a different way. The culture we grew up in influences how we look at ailments (3) and the way we handle pain (2). It is through Pathographies that these worlds of illness and health are brought together, creating a narrative that allows us to delve inside the patient’s mind regardless of ethnicity or race. We look beyond the clinical terms, the graphs and the numbers, and not only does this help us to see the patient through a broader lens, it also breaks barriers with the next person we meet. This cultural understanding allows us to look after the ill in the way that they want to be treated – with dignity and compassion. It puts control back in the person’s hands at a time when chaos reigns. Pathographies can help to break the formulaic clinical story. A person is not a machine with a broken part, but an autonomous being with desires and goals, whose need for help cannot always be fit into a category.
All too often we can get caught up in the stereotypes: the smoker with COPD, the teenage overdose, the forty-year-old female with gallstones. We must remember our own biases as we sit in our staffrooms: our own assumptions built from our privileged educations. We no longer live in the world of the authoritative doctor dressed in his white coat. Instead, we let the patient’s words fill the silence.
Instead of opening another lengthy medical textbook, looking up the obscure and the malignant, we can open up a Pathography and step into our patients’ lives. No matter what our role, whether it’s inside healthcare or not, the voice of illness speaks in everyone’s ear and it deserves to be heard.
Further Reading
Illness as a Metaphor, AIDS as a Metaphor by Susan Sontag
An Unquiet Mind by Kay Redfield Jamison
C: Because Cowards Get Cancer by John Diamond
Intoxicated by My Illness by Anatole Broyard
References
1. American Association for Marriage and Family Therapy. 2014. Chronic Illness [Online]. Available at: https://www.aamft.org/iMIS15/AAMFT/Content/consumer_updates/chronic_illness.aspx [Accessed: 28th October 2014]
2. Briggs, E. 2008. Cultural perspectives on pain management. Journal of Perioperative Practice. 18:468-471
3. Wedel, J. 2009. Bridging the Gap between Western and Indigenous Medicine in Eastern Nicaragua. Anthropological Notebooks. 15:49-64
Featured image:
by Personal Kaleidoscope