Each year there are many medical conferences held around the world. These could be conferences about new research, medical education or, perhaps, a gathering of those in a specific specialty. Last year I was lucky enough to attend the American Medical Women’s Association (AMWA) Centennial Conference in Chicago, IL. After attending my first medical conference, I have made it a personal goal to attend at least one each year.
So, was it worth it? In my opinion, it is a definitive yes. I’ll break down some of the pros and cons based on my experience so you can decide for yourself if you’ll be attending a conference (or two) within your medical school years.
Pros
- Connections. I can’t go on long enough about how many new connections I made. I met physicians from around the nation in different specialties. I heard from speakers who had written books, gotten double board certified while raising a family of four, and even travelled to the moon (I’m not kidding, Mae Jemison was in attendance). An easy way to stay in touch with the new colleagues you’ve met is LinkedIn. After hearing from them at the conference I connected with them on LinkedIn, which allows me to see what they are doing professionally and keep them in my network for any future communications.
- Relationship growth within my organization. The AMWA chapter at my medical school has always been a tight-knit group, but this trip made many of us even closer. It was a great way to get the entire group motivated for an awesome upcoming year. We were able to bond over our favorite speakers and chat about some of the important issues being discussed on the women’s rights front.
- Stepping outside of your comfort zone. In advance, the conference paired student attendees with physicians and asked students to meet with and interview the physician. I ended up getting paired with an internal medicine physician coming from the renowned Tuft’s University. I was intimidated at first because she came from such a prestigious university, but she turned out to be incredibly down to earth and friendly. I had the opportunity to talk to her about her personal journey and how being a woman in a once male-dominated field affected her. She told me a story of when she was involved in a patient’s care when they began coding. As if this weren’t stressful enough, she was seven and a half months pregnant and started having contractions. Womanhood presents unique obstacles, but this physician was able to overcome them with flying colors.
- Exploring a city! The conference allowed me to experience Chicago in a new way. We stayed right in the heart of downtown and went on quite a few sight-seeing adventures. Next year the AMWA conference is in Miami, which would be so much fun to visit! Heading out of town for a conference can feel like a mini vacation from the hectic life of a medical student.
- Intellectual growth. The AMWA conference placed a strong emphasis on the advancement of women in medicine. We heard from numerous female physicians about their experiences within the field and how they got onto their current path. It was empowering to listen to women who had written numerous books, founded various organizations and impacted society so greatly. Additionally, I was able to hear from numerous female physicians about raising a family and having their dream career. It gave me hope that the life I want is doable. I think this conference truly revitalized my energy after a long first year in medical school. It allowed me to see past the current grueling coursework to what my career could potentially blossom into.
- Money. Okay, to be honest, this AMWA conference was actually affordable, but I know many are super pricey. My advice is to seek funding from various sources. This year I’d really like to go to the conference again, so I plan to set up a Go Fund Me account that will allow my relatives to donate some money to help me attend. Last year, I was fortunate enough to get some money to support my travel. Most student organizations can get some funding from their school, which is what our AMWA group was able to do. In addition, many conferences have grants or scholarships to help students attend. I recommend looking at a few different conferences you find interesting and pick one that is the most economical. Another option is to create a poster (or research) to present and most likely you can get a grant from your school to present it at a conference.
- Time. The conference I went to was an entire weekend event, so I wasn’t able to study at all. In the little down time we did get, I wanted to explore the city or just relax for a few minutes. Plan ahead and study during the car (or plane) ride. Check your schedule and make sure the conference falls during a time that isn’t incredibly hectic for you. Even though conferences are a large commitment, the time “lost” I think ends up being an overall gain when you consider the benefits.
Conférence NWX2012 by Frédéric BISSON


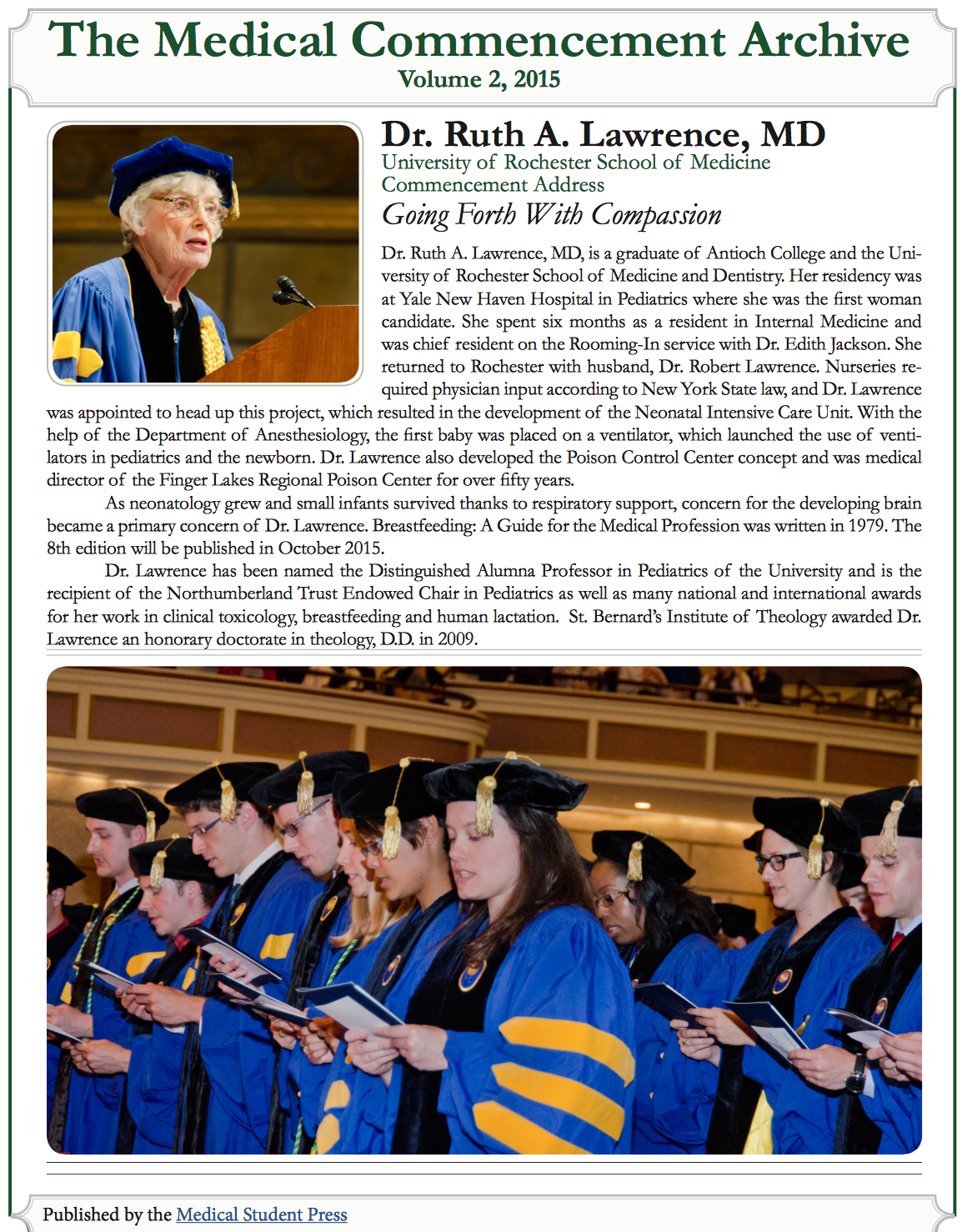
 Dr. Myron Cohen is known for his invaluable contributions to the construction of the HIV Prevention Trials Network 052, which established that treating an HIV patient with antivirals makes them less contagious to their sexual partners.
Dr. Myron Cohen is known for his invaluable contributions to the construction of the HIV Prevention Trials Network 052, which established that treating an HIV patient with antivirals makes them less contagious to their sexual partners. Bill McRaven, who recently retired as a four-star admiral after 37 years as a Navy SEAL, became Chancellor of The University of Texas System in January 2015.
Bill McRaven, who recently retired as a four-star admiral after 37 years as a Navy SEAL, became Chancellor of The University of Texas System in January 2015.